Susan E. Brown, PhD.
Myth 1: Lack of calcium causes osteoporosis.
Yes, calcium is important, but it’s a myth that simply taking a high amount of calcium will guarantee bone health. To protect your bones, you need enough of 19 additional essential bone nutrients, not just calcium. For example, without enough vitamin D, your body only absorbs about 10- 15% of the calcium from your diet, but when you take enough, the absorption rate jumps to 30-40%. Other critical nutrients for bone health are vitamin K, magnesium. manganese, zinc, copper, strontium, boron, vitamin C, vitamin B12, and folic acid.
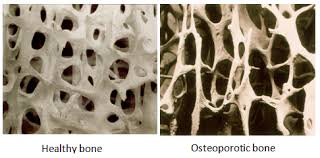
Myth 2: Osteoporosis is normal; as your bones age they should get weak.
One of the most dangerous bone health myths is that osteoporosis is inevitable as we age. While there are some fixed risk factors — such as our age and gender — you can control most of the risk factors that lead to excessive bone loss, osteoporosis, and fracture. The truth is, you can maintain and rebuild strong bones at any age.
Myth 3: A diagnosis of osteoporosis means you’ll suffer a fracture.
Research shows that the vast majority of those who fracture do not have an “osteoporotic” bone density; they have either osteopenia or normal bone density. Real facture risk depends not on bone density, but on one’s “total load” of bone-weakening risk factors.
Myth 4: You don’t need to worry about osteoporosis until menopause.
Bone loss — even osteoporosis — can be secretly affecting you in your 20s, 30s, and 40s. We normally achieve peak bone mass in our 20s and then begin to lose it, some of us more quickly than others.
Myth 5: There’s nothing you can do once you have osteoporosis other than take a drug.
The U.S. Surgeon General recommends much more than drugs! The first steps are the natural approach to bone health combining nutrition, physical activity, and fall prevention. Next comes assessing and treating the underlying causes of compromised bone health. Finally, bone drugs are listed as a last recourse.
Myth 6: There aren’t any signs or symptoms of bone loss.
While many women don’t realize they have a bone issue until they fracture, there are early signs and symptoms of bone loss. These include receding gums; decreased grip strength; weak and brittle fingernails; cramps, muscle aches and bone pain; height loss and low overall fitness. Another good way to know if you are losing bone is to test your first morning urine pH level to see if your body is too acidic. Metabolic acidosis can deplete your bone mass systematically. Alkalizing through diet and supplements preserves bone.

1 You’ll put your bones at long-term risk.
Bone drugs have troubling side effects that can significantly affect your bone health, especially when used over time. One troubling side effect is seen with bisphosphonate drugs. While they may halt bone breakdown in the short term, after about a year, these bone drugs also halt bone building — leading to brittle bones that may be more susceptible to fracture, not less. How’s that for irony?
2 There are risks to your whole body.
Serious consequences like stomach irritation, heightened risk of esophageal cancer, blood clots, leg cramps, vision changes, nausea, vomiting, or constipation. These side effects are critically important to consider, especially if you’re being asked by your doctor to take bone drugs for what may be normal bone loss or even as prevention.
3 Bone drugs produce few lasting results.
Popular bisphosphonate bone drugs “work” by temporarily creating bone mass from drug molecules, but they don’t offer lasting results. Based on my experience, I’ve learned that just because bones may look denser on a bone scan, it doesn’t necessarily mean they are measurably stronger. What’s more, the recommended limit for taking bone drugs safely is just five years, at which time any “benefits” of bisphosphonates disappear.

Why is it important to identify and treat osteoporosis?
It can lead to fracture of the long bone, femur.
Speaking at the centennial annual meeting of the Clinical Orthopaedic Society, Erika J. Mitchell, MD, said “Hip fractures kill. The 30-day mortality rate after hip fracture is about 9 percent. It rises to 17 percent if the patient , already has an acute medical problem. If a patient has heart failure while being treated for a hip fracture, the 30-day mortality increases to 65 percent. And if a patient has pneumonia after a hip fracture, the 30-day mortality increases to 43 percent.”
And in the year following hip fracture, mortality is 20%. Hip fracture reduced life expectancy by 1.8 years or 25% compared with an age- and sex-matched general population. About 17% of remaining life was spent in a nursing facility. One year after a hip fracture, only approximately 40% of surviving patients regain their previous level of mobility and only approximately 25% regain their former functional status.

The takeaway?
Consume calcium from food sources. Supplement with a calcium containing magnesium and Vit D too.

Exercise, especially weight bearing exercise strengthens bones and muscles, preventing falls and improving balance.

Eat sensibly, supplement where necessary.

Stay Healthy!


